Skin is our largest and most visible organ, which is why it’s important to know more about it. Skin lesions are bumps, spots, or unusual blemishes that can develop on the skin. There are different types of skin lesions and each may require specific treatment. It’s important to know the difference between normal and abnormal lesions to avoid making a misdiagnosis. Skin lesions are the result of a disease in the top layers of skin. Most are benign (non-cancerous) but some can be malignant (cancerous).
Our skin is our first line of defense against any disease or infection. The skin can show signs of wear and tear from daily activities, such as growths or marks. These skin lesions are unique and each person has a different treatment. However, diagnosis is only half the battle. Each skin condition must be referred to a dermatologist.
Table of Contents
What are skin lesions?
A skin lesion refers to a skin area that is abnormally growing or appears in comparison to the surrounding skin.
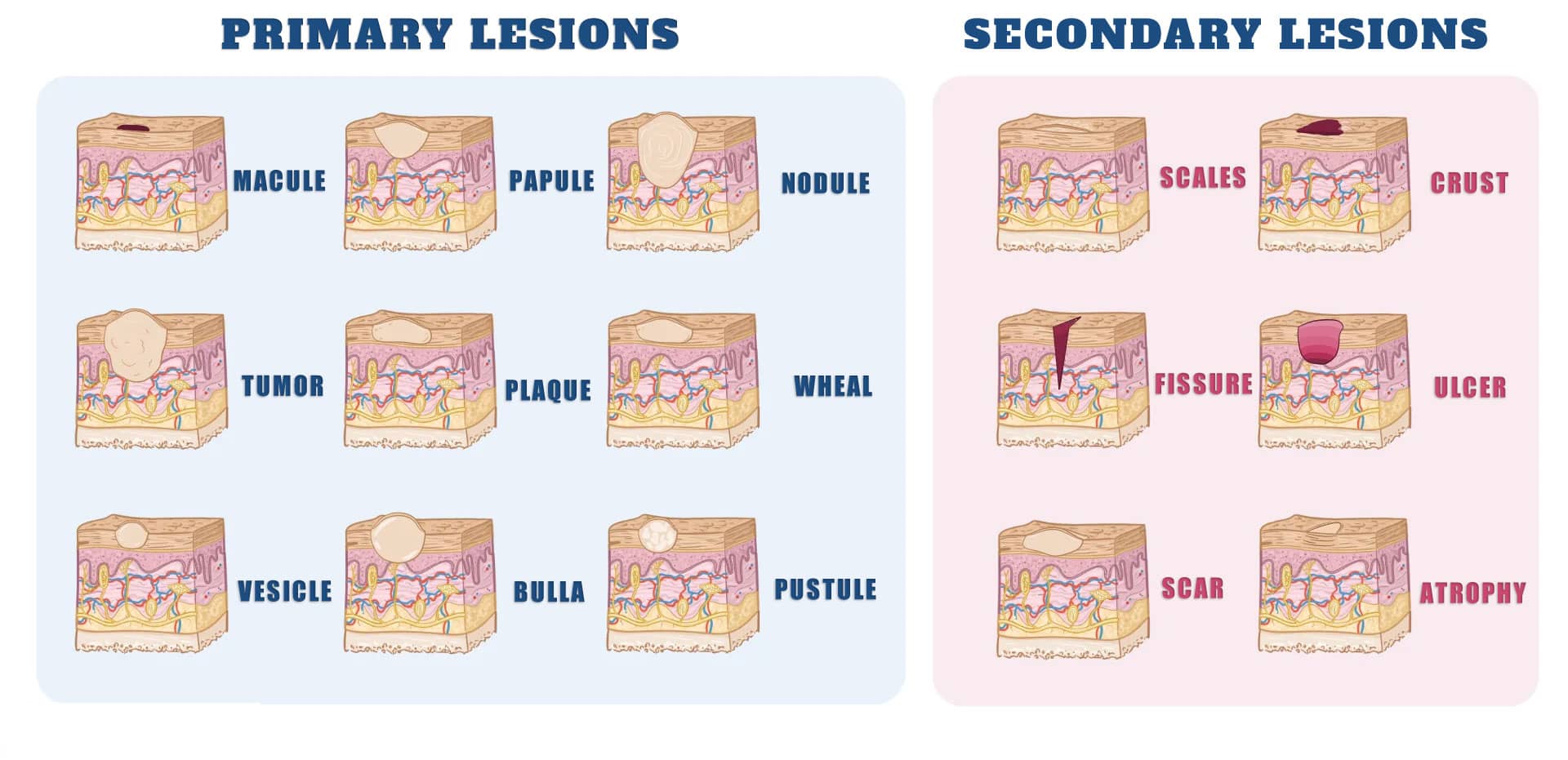
There are two types of skin lesions: primary and secondary.
Primary skin lesions can be a result of inherited or acquired skin conditions.
Secondary skin lesions can result from primary skin lesions that have been irritated, or otherwise manipulated. A secondary skin lesion is when a primary skin lesion is irritated or manipulated.
Premalignant Lesions Of Skin
Malignancy is the main concern for unusual skin lesions. Moles can be a sign of melanoma or other forms of skin cancer. A professional dermatologist is the best way to diagnose it, but there are other signs you can look for.
- A lack of symmetry (normal moles look perfectly round or oval).
- A rise in elevation above the skin’s surface
- Bleeding and scab formation
- Color changes or three different shades of brown, black
- Itchiness and inflammation
- With irregular edges, the shape of the object changes
These indicators can be used as a guideline for skin lesions. A dermatologist will inspect the lesion and ask about your medical history. In most cases, they will also perform a scrape or a swab to determine the source of infection.
The distribution and location of skin lesions
It is important that you note whether:
- Distribution can be random or pattern, symmetrical or asymmetric.
- Lesions can be found on either sun-exposed skin or protected skin.
- Multiple lesions can be made.
- Somebody parts may be affected, such as the palms and soles, scalp, mucosal membranes, or scalp.
While not all patterns can be considered pathognomonic they do indicate certain diseases.
Psoriasis can often affect the scalp, and extensor surfaces at the elbows and knees as well as the umbilicus and gluteal cleft.
Lichen planus is a common condition that appears on the wrists and forearms.
Vitiligo can be isolated, patchy, or grouped around the distal extremities and the face, especially around the eyes.
Discoid Lupus Erythematosus is characterized by lesions on sun-exposed skin, particularly the forehead, nose, and conchal bowl of each ear.
Hidradenitis Supurativa is skin with a high concentration of apocrine cells, including the axillae, and under the breasts.
Color
Health care professionals should be aware that skin color can affect the appearance of colors. Cutaneous tumors can be pink or red. Red may be seen in superficial vascular lesions, such as port-wine staining.
Hypercarotenemia is a benign condition in which carotene has been deposed after excessive dietary intake of beta-carotene. This causes orange skin.
Yellow skin is a sign of jaundice and xanthelasmas, pseudoxanthoma Elasticum, and xanthomas.
Green fingernails suggest Pseudomonas Aeruginosa infection.
The cause of violet skin could be cutaneous hemorrhage, vasculitis, or both. Purple can be caused by vascular lesions and tumors such as Kaposi Sarcoma or hemangiomas. Dermatomyositis is characterized by a lilac-colored eyelid or heliotrope eruption.
The skin can develop shades of blue, silver, and gray due to the presence of drugs or metals, such as minocycline, amiodarone, and silver (argyria). The color of ischemic skin can range from purple to gray. Deep dermal nevi appear blue.
Melanocytic skin lesions, which include nevi or melanoma, may appear as black spots. Black eschars can be a collection of dead skin cells that may result from infection.
What causes skin lesions
An infection of the skin is the most common reason for skin lesions. A wart is one example. One example is a wart. The human papillomavirus, which causes warts in humans, can be passed directly from skin-to-skin contact.
Direct contact is another way to transmit the herpes simplex virus. This virus causes cold sores as well as genital herpes.
Systemic infections, which are infections that affect your entire body, can cause skin inflammations all over your body. Chickenpox, shingles, and others are two examples. MRSA and cellulitis, which can be life-threatening infections, involve skin lesions.
Some skin lesions such as freckles and moles are genetic. Birthmarks are lesions that were present at birth.
Other reactions can result from allergic reactions, such as contact dermatitis and allergic eczema. Poor circulation and diabetes can cause skin sensitivity, which can lead to lesions.
Because of the wide range of lesions, there will be many causes.
- Most skin lesions are caused by bacterial, viral, or fungal infections, and sometimes parasitic transfer.
- The symptoms of allergies or sensitivities can cause lesions.
- Marks and bruising can be caused by certain health conditions, such as diabetes or liver disease.
- Like most skin conditions, genes play an important role in the development of skin conditions such as freckles or moles.
- Severe health issues such as skin lesions (e.g. skin cancer) via growths.
Different types of skin lesions
There are many types of skin lesions. It can be hard to identify the cause. There are some common characteristics that will help you pinpoint the problem.
Itchy, red, and inflamed skin is a sign of an allergic reaction. It could also be caused by a fungal infection if the lesion becomes large and scaly. If the lesion appears to be crusted or filled with pus it could be a bacterial infection.
Skin lesions refer to abnormalities in the skin that are not normal for the surrounding tissues. They can be acquired or born.
There are many types of skin lesions. Some skin lesions are benign and are therefore harmless. Some can be very serious. They can appear anywhere on your body or in just one area.
You can also vary the shape. Some lesions are symmetrical. This means that they have the same shape throughout. Some lesions are irregular in form.
It is possible to identify skin lesions by the way it looks and how it appears. Doctors consider the following factors when diagnosing a skin lesion:
- Color
- Size
- Texture
- Localization
Let’s examine different types of skin conditions, their causes, and their treatment.
Primary vs Secondary Lesions
Primary and secondary skin lesions can be classified as either primary or secondary. Primary skin lesions can develop over time or they may be present at birth.
Primary skin lesions can lead to secondary skin lesions. If a primary lesion is present, secondary skin lesions can occur.
- Disturbed
- Are you feeling upset?
- Time changes
A crust can form if the skin is scratched. This is called a secondary lesion.
Types of skin lesions chart
One of the most common reasons patients see their dermatologist is because they have skin lesions on their bodies. Skin lesions occur as a result of cancer or benign tumors, or as a result of infectious diseases such as herpes and chickenpox.
Skin lesions are also commonly caused by cosmetic procedures such as laser hair removal, botox injections, and chemical peels. No matter what type of lesion you may have, it is important to know what the underlying cause is so that you can seek the appropriate treatment.
It is difficult to detect skin cancer early because some of the symptoms are similar to those of other skin conditions. For example, some skin cancers have a waxy or pearly appearance, which can look similar to a scar or freckle. However, you can use a skin lesions chart to help you identify suspicious growths, lesions, or moles.
Primary skin lesions
Primary skin lesions are usually divided into three groups:
- Flat lesions. These include patches and macules.
- Fluid within the skin layers can cause lesions. Vesicles and pustules are two examples.
- Solid masses are lesions. Nodules and tumors are two examples.
Primary lesions are classified as:
- A plaque is a lesion that looks like a papule, is larger than 1-2 cm (0.4-0.8 inches), and is raised like one. It can be flat-topped, rough, and solid.
- A vesicle is a fluid-filled blister that measures less than 0.5 cm (0.2 inches) in diameter.
- Cyst: An area of skin raised above the surface and filled with fluid, semi-solid or liquid fluid.
- Bulla: A vesicle with a diameter greater than 0.5 cm (0.2 inches), and filled with fluid.
- Macule: A flat, irregularly colored lesion less than 0.5 cm (0.2 inches).
- Nodule: A round, raised, solid bump that is greater than 0.5 cm (0.2 inches).
- Papule, also known as maculopapular, is a solid lesion that can grow to up to 0.5 cm (0.2 inches) in size. It is clear and firm with no borders. It can be found in many colors.
- Patch: A flat, solitary lesion with a color change and greater than 0.5 cm (0.2 inches).
- Pustule: A vesicle-like structure, but it is filled with pus.
- Telangiectasia – Clusters of “spider veins” where tiny blood vessels cause red marks on the skin.
- Tumor: A tumor is a lesion larger than 0.5 cm (0.2 inches). It looks like a nodule but has a greater size. Tumors may be benign or cancerous.
- Wheal is an irregularly shaped, solid, elevated area that can vary in color but lasts only a brief time.
Primary lesions are caused by specific causes and occur when the skin reacts to an external or internal environment. Fluid within the skin layers can cause pustules, bullae, and vesicles. Plaques, nodules, tumors, and papules can be felt as solid, elevated masses.
Primary skin lesions can be either those that you were born with or those that you develop over time. They can be fluid-filled, flat, or solid.
As are moles, acne, and birthmarks are primary skin lesions.
The following are other types:
Blisters
Blisters are skin lesions that have been filled with a clear liquid. Vesicles are small blisters less than 1 cm. Bullae, or simply blisters, are larger blisters.
A blister is an area of fluid that forms between two layers of skin. Blisters are usually caused by something rubbing against the skin. However, they can also occur due to other causes. Even if they aren’t serious, most blisters can be quite painful.
It is best to let a blister heal naturally. Only in rare cases is it appropriate to pop a blister. Doing so could lead to the spread of bacteria. Proper technique and hygiene are essential to prevent infection.
These lesions could be caused by:
- Burns
- Friction injuries such as shoe bites
- Cold (extremely low temperature)
- Reaction to irritants
- Drug reactions
Types of Blisters: There are several types of blisters, each is caused in different ways.
- Blood Blisters
- Friction Blisters
- Blisters on the Feet
- Heat Blisters
- Health Conditions
Macules
A macule (or macule) is a discolored, flat area of skin that is less than one centimeter in width. It does not affect the skin’s thickness or texture. Patches are defined as areas of discoloration greater than or equal to 1 cm.
Some conditions, such as vitiligo, are marked by patches or macules on the skin that are lighter or whiter than others.
Flat lesions less than 1 cm are called macules. You can identify them by looking at them and touching their skin. A macule is defined as a lesion that’s not raised or less than 1 cm in diameter.
Depending on the cause, a macule may be any number of colors. Macules may be either mole, which is darker than the skin, or vitiligo lesions, which are hypopigmented (or lighter) relative to the skin.
The term rash refers to a series of changes in the skin. Rashes may have patches, macules, papules, or raised skin lesions less than 1 cm. Plaques (raised, raised skin lesions less than 1 cm) are all possible.
Doctors use the term “macule” to describe skin conditions. A dermatologist is recommended if you have a flat, less than 1 cm-wide skin lesion and wish to determine the cause.
Macules can be caused by the following conditions:
- Vitiligo
- Moles
- Freckles
- Sunspots, liver spots, and age spots
- Post-inflammatory hyperpigmentation is a condition that occurs after the healing of acne lesions.
- Tinea versicolor
Nodules
A nodule is a growth of abnormal tissue. Nodules may form just below the skin. They may also form in deeper tissues and internal organs. Nodules are a term dermatologists use to refer to any lump under the skin that is at least one centimeter in diameter.
There are two types of nodules: dermatofibroma and pyogenic granuloma. Nodules can form on the tendons or muscles of the body in response to injury. They are often found on the vocal cords. They can form in the thyroid or lung or in other medical conditions like rheumatoid or rheumatoid.
A growth, lump, or tumor that could be malignant (cancer), or benign (not necessarily cancer).
Inflammation can be caused by infections that affect the lungs such as tuberculosis and fungal infections. Inflamed areas may develop a cluster of cells known as a granuloma, which can give the appearance of a nodule.
A nodule can either disappear on its own or remain the same size. To monitor the growth of the nodule, patients treated in this manner should see their doctor at least once every six months. There is usually no reason to be concerned as long as the nodule doesn’t grow.
They are not cancerous and won’t spread. They can shrink or stop growing slowly. Don’t often pose a threat to your life They don’t usually need to be removed.
Due to the severity of acne nodules (scarring), they will not disappear within a few days. Professional evaluation and treatment are often required in order to prevent future scarring. This severe breakout can last for up to six weeks.
Papules
A Papule refers to a raised area of tissue in the skin that is less than one centimeter wide. A papule may have distinct or indistinct boundaries. A papule is a small, raised bump on the skin.
This is caused by excess oil or skin cells that clog a pore. Papules do not have visible pus. The papule will usually fill with pus within a few days.
Papules, like most forms of acne, can cause an increase of oil and germs in the pores caused by dead skin cells. Papules are usually caused by a blockage of pores that causes a hair follicle becomes swollen.
Papules are slightly larger than whiteheads and blackheads. They form a bumpy, raised dot instead of a small dot.
Although they may be white or yellowish in color, they can form a raised bump without a defined head. Papule popping, unlike pustules, should not be attempted as it can cause irritation and worsen the problem.
This will clear up acne blemishes. Wash your face with an acne facial wash that contains salicylic acid or benzoyl peroxide twice daily. A dermatologist may be able to help you if there are a lot of pimples.
Pustules
A pustule refers to a large, yellowish-colored lump of skin with pus. It is basically a large pimple. Pustules can be caused by a variety of conditions, including acne and the once-deadly smallpox disease.
These cells are present when there is an infection or your body is trying to fight it with white blood cells. This can lead to a mix of infected fluid (pus) and dead white blood cells (dysfunction).
Pustules can develop when pus builds up in the pore or under the skin.
Should be careful with nasal vestibulitis, or nasal folliculitis. This is a rare bacterial infection of the nostrils. Symptoms of this disease can look like pustules or other common pimples inside the nose. It usually develops when the hair follicles become infected, such as after a person picks or plucks nose hairs.
Pustules can occur in a variety of conditions:
- Acne is A very common skin condition that causes pustules larger than normal pimples. These occur when your skin’s pores become so irritated that their walls crack.
- Psoriasis This skin condition causes itchy, red patches. Acute pustular psoriasis can be caused by stress, infection, medications, or certain chemicals.
- Rosacea This skin condition causes reddening of the skin and pimples. However, inflammatory rosacea, a type of disease that can cause pustules, is possible.
- Chickenpox This disease in childhood and others caused by a similar virus can cause skin lesions that turn into pustules with time.
- IgA pustules: Pustules can also be a sign of this rare condition that causes your immune system to attack itself.
- Smallpox – Pustules are one of the most visible signs of this deadly disease, which has claimed millions of lives in the past century. It is no longer a threat thanks to a vaccine. However, samples of the virus remain in laboratory facilities in the United States as well as Russia.
Rashes
A rash refers to a visible change in your skin’s texture or color. Itchy skin can cause itching, scaly, bumpy, or other irritations.
Rashes can be caused by many things. Here are the top 21 causes of rashes:
- Flea bites
- Fifth disease
- Rosacea
- Impetigo
- Ringworm
- Contact dermatitis
- Allergy eczema
- Hand, foot, and mouth diseases
- Diaper rash
- Eczema
- Psoriasis
- Chickenpox
- Systemic lupus erythematosus (SLE)
- Cellulitis
- Drug allergy
- Scabies
- Measles
- Tickle!
- Seborrheic eczema
- Scarlet fever
- Kawasaki disease
Contact dermatitis, one of the most common causes of the rash, is the most common. Contact dermatitis is a condition in which the skin comes into contact with a foreign substance.
This can cause a rash. Itchy, red, or inflamed skin may result. Contact dermatitis can be caused by:
- Laundry detergent, soaps, and beauty products
- Clothing dyes
- Contact with rubber, elastic, and latex chemicals
- Poisonous plants such as poison oak, poison sumac, and poison ivy can be touched.
Rashes can also be caused by taking medications. They may develop from:
- Allergic reaction to the medication
- Side effects of the medication
- Photosensitivity to medication
Other causes
The following are possible causes for rashes:
- Sometimes, a bug bite can cause a rash. Because tick bites can transmit diseases, they are especially concerning.
- Atopic dermatitis or Eczema is a form of a rash that occurs mostly in those with allergies or asthma. Itchy, reddish-colored, and often with a rough texture. Eczema can result in a blister or rash behind the ear that is extremely itchy, red, and inflamed and that often
- Psoriasis, a common skin condition, can lead to a red, itchy, itchy rash that forms along the scalp, elbows, and joints.
- The seborrheic epidemic, which is most commonly affecting the scalp, causes redness, scaly spots, and dandruff. It can also affect the ears, nose, mouth, and throat. It’s also known as a crib cap.
- Lupus erythematosus, an autoimmune disorder that causes a rash on the nose and cheeks, is called Lupus erythematosus. This rash is also known as the “butterfly” or malar rash.
- Rosacea is a skin condition that can last for years. Rosacea can be of many types, but they all have the same symptoms: redness on the skin and rash.
- Ringworm is a fungal infection that results in a distinctive, ring-shaped rash. Jok itch, athlete’s foot, and scalp ringworm are also caused by the same fungus.
- Diaper rash is a common skin condition in toddlers and infants. This is usually caused by too much time in dirty diapers.
- Scabies refers to mite infestations that live on your skin and burrow into it. Itchy, bumpy skin can result.
- Cellulitis refers to a bacterial infection that affects the skin. Cellulitis is a bacterial infection of the skin that causes redness, swelling, and pain to the touch. Cellulitis can become serious if it is not treated.
Wheals
An itchy, raised area of skin (pruritic), that can sometimes be a sign of an allergy. A weal (or wheal is a superficial, pale-colored, or erythematous skin swelling. It can last from a few seconds to 24 hours. Angioedema, which is deeper swelling of the skin or mucous membranes, can be co-existing with urticaria.
This is the grade level according to the word’s complexity. A small, itchy, or burning swelling of the skin. This could be caused by a mosquito bite or hives. A welt or wale.
Your body releases histamines and other chemicals when you have an allergic response to a substance. Itching, swelling, or other symptoms can result. Hive is a common reaction. Hives are common in people with hay fever or other allergies.
Wear loose-fitting cotton clothes. Use ice cubes wrapped in a cloth to apply a cold compress to itchy skin unless you have hives. The anti-itch medication you can purchase without a prescription such as an antihistamine and calamine lotion.
Secondary skin lesions
Secondary skin lesions include scales and crusts, excoriations, ulcers, and fissures scars. Scales are dead cells from keratinized cells that have been shed. They can be found in eczema and psoriasis. They are irregular, flaky, and vary in size. They can be silvery, tan, or white and can be thick, thin, or oily.
Secondary lesions are lesions that have been modified by the primary lesion by the person with it or by natural evolution.
Secondary skin lesions are:
- Atrophy is a condition where the skin becomes thin, transparent, and wrinkled. This is often caused by the use of topical medicines like steroids.
- Crust: The dried fluid’s rough and elevated surface. It could be pus, blood, or serum.
- Erosion is the loss of the skin’s top layer. It appears moist and glistening.
- Excoriation is a straight scratch that causes the skin’s top layer to be removed.
- Fissure: A series of cuts in the skin that extend beyond the top layer and reach the second layer. Fissures can be very painful and can be caused due to excessive dryness.
- Lichenification is a rough thickening or thinning of the skin’s top layer.
- Maceration is skin that is dry, wrinkly, and lighter in color. This occurs when the skin comes in contact with fluids or water for too long. This can be caused by poorly cared-for leaking wounds.
- Phyma is a thickening of the skin. This is common in advanced rosacea.
- Scale: A buildup of cells that forms patches and then peels off the skin.
- An ulcer is a deep cut that penetrates the skin’s second layer. It can be concave or variable in size. More severe ulcers can result.
- Umbilication is a dip in a skin lesion that looks like a navel.
Secondary lesions are lesions that occur when the primary lesion is modified by the patient or the environment.
Primary lesions can lead to secondary skin lesions. These lesions usually occur when primary lesions are disturbed, irritated, or change over time.
Primary skin lesions can become secondary skin lesions if they are inflamed.
These are the most common secondary skin conditions:
Crusts
The Crust is an area slightly raised in size and made up of blood, dried serum, or purulent exudate. Excoriation – linear scratching that may or not is removed. Lichenification–rough, thickened epidermis; accentuated skin markings caused by rubbing or scratching (eg, chronic eczema and lichen simplex)
Dry skin exudate, such as serum, blood, pus, or a mixture. Crusts can be seen in conditions with a pustular component, such as canine pyoderma and pemphigus fetus.
Plaques on the skin are caused by Psoriasis. This is an autoimmune condition that occurs when your immune system overreacts. Instead of shedding, your skin cells accumulate.
Scales
Scales are a visible peeling or flaking of outer skin layers. These layers are called the stratum corneum.
Scaling of the skin can be a sign of many medical conditions such as psoriasis and contact dermatitis. If left untreated, some causes can cause serious health problems. The most common areas affected are the hands, legs, and face.
Scales are caused by the outermost layer (the epidermis) becoming dry and flaky. Scaly skin is caused by a buildup of dead skin cells. Scales may be thin and fine like pityriasis pinka or thicker than psoriasis.
Scaling skin refers to the loss of the outer layer in large scale-like flakes. Although the skin may appear dry and cracked, it is not always due to skin dryness. Desquamation is another name for scaling skin.
Most dry flaky patches on the skin of your face are not serious and will disappear over time. Dry patches may indicate something more serious. If dryness persists or is itchy, consult your dermatologist. If you are unsure of the cause, it is important to consult a doctor.
These acids are applied to the skin and weaken the bonds between cells. The outer layer of the skin is affected by this process, and it causes it to shed. This softens and eliminates scales. These acids can be found in creams, lotions gels, ointments foams, shampoos, and gels.
Scares
Permanent fibrotic changes to the skin result from tissue injury. Normal tissue is replaced with fibrous connective tissue at the site of injury. Scarring can be hypertrophic or sclerotic due to collagen proliferation, or atrophic. The pattern of healing in the affected region.
Scarring caused by cuts, scratches, or other injuries may leave scars that are not easily replaceable with healthy, normal skin. Instead, the skin will show a thickened, raised scar. This scar is called a keloid.
Atrophy of the skin
General skin atrophy is which refers to a decrease in epidermal thickness and dermal thickness, regressions of the sebaceous and subcutaneous fat losses, and muscle-layer loss. These changes usually occur after 2 to 3 weeks of moderate-to-high-potency topical corticosteroid treatment.
Aging causes the majority of thin skin. Along with wrinkles and furrows, thin skin is an inevitable part of growing older. Skin that is dry and easily damaged is also a common cause. The sun plays an important role in the skin’s thinning process. UVA and UVB rays may damage or kill skin cells.
While the short-term treatment for skin atrophy can still be reversed; the long-term, which causes striae to develop, is permanent.
Cutaneous atrophy clinically refers to wrinkled, shiny, and telangiectasia-like pseudo scars, striae, hypopigmentation, or prominent deep veins.
Multiple treatments have been reported for steroid-induced skin atrophy. These include fat-grafting, surgical excision, and pulsed-dye Laser.
General skin atrophy is characterized by a decrease in epidermal thickness and dermal thickness, regressions of the sebaceous and subcutaneous fat losses, and muscle-layer atrophy.
These changes typically occur after 2 to 3-week of moderately-to-high-potency topical corticosteroid treatment.
Ulcers
Ulcers can be sores on your stomach or small intestinal. Your esophagus (throat) could also be affected by ulcers. Most ulcers are found in the small intestine. These ulcers are known as duodenal ulcers.
Pressure sores are a common form of skin ulcer. The continuous pressure placed on skin areas can cause them to become damaged. This is usually caused by a person being unable to move well. Check out the separate leaflet Pressure Sores. These skin ulcers are known as malignant skin ulcers.
Skin ulcers can be identified by the following symptoms:
- A foul odor is detected in the vicinity
- Clear, bloody, or pus-filled drainage from the ulcer
- Discoloration of skin
- Hair loss in the vicinity of the ulcer
- Itching
- Scabbing
- Swelling of the skin around the ulcer
- The area around the ulcer should have dry or flaky skin
- Tenderness or pain near the affected area
Over-the-counter medicines to treat ulcers can be found at your local pharmacy. There are many medications available that can help ease pain and speed up the healing process, including antacids and digestive tract-fortifying drugs like Pepto Bismol. OTC drugs such as antacids may reduce pain from an ulcer but should not be considered a substitute for medical attention.
How are skin lesions diagnosed?
A dermatologist or doctor will perform a complete physical exam to diagnose a skin condition. A doctor will conduct a complete physical exam to determine the cause of the condition. Doctors can identify the cause by assessing the appearance, size, location, color, and texture of any bumps, blisters, or rashes. You may also find other symptoms that are not related to skin conditions.
A variety of tests will be performed by your dermatologist or GP to diagnose your skin condition.
These include:
- Skin biopsy
- Blood test
- X-rays
- MRI/CT scans
- Allergy testing
- Swab (taken from sensitive areas, e.g. the mouth)
Not to be forgotten, a physical examination of any skin complaints. These tests can be used to diagnose most medical conditions. They have been proven to be very efficient and are well-researched.
Your GP and dermatologist will both examine you and ask questions about your health and symptoms. This is a good time to be open and honest. If you know someone who has the same skin condition, please tell them.
This is vital as many skin conditions can be passed down from one generation to the next. This could be the reason for your condition. The final diagnosis is either confirmed or rejected.
The first step in diagnosing skin lesions is a careful physical exam and medical history. The physical examination includes assessing the color and comparing it with other lesions. Dermoscopy is a method of examining skin lesions with a magnifying lens. To evaluate certain skin conditions, a Wood’s lamp examination can be performed under black light. To aid in the diagnosis, some aspects of the medical history, such as sun exposure, allergies, and current medication, can be very helpful.
Additional diagnostic tests may be required for some skin lesions. These include blood tests, allergy testing, skin or wound swabs to conduct microbiological investigations, and imaging techniques such as an X-ray or CT scan. A biopsy may be done if the diagnosis remains unclear or malignancy is suspected.
They may take skin samples or a biopsy to confirm the diagnosis.
How are skin lesions treated?
The underlying cause of skin lesions is what will be treated. Your personal history and previous treatments will all be considered by a doctor.
Many of these lesions (including cold sores or blisters) usually disappear within a few days. Some, like eczema or psoriasis, are chronic conditions that require ongoing treatment. Doctors can often treat lesions that could become cancerous.
You can treat benign skin lesions with topical medication, such as retinoids or corticosteroids, or antimicrobial agents. This includes laser therapy, cryotherapy, and phototherapy. The underlying cause of the skin lesions may be addressed with treatment.
Medications
Topical medication is often used first to treat inflammation and protect the area. The skin lesion may also cause mild symptoms such as itching and burning.
You may be prescribed oral medication to ease skin lesions if your skin is affected by a systemic infection such as chickenpox, shingles, or other diseases.
Surgery
To treat and relieve infected skin lesions, it is common to have them pierced and drained.
If suspicious-looking moles have been developing over time, it may be necessary to remove them surgically.
Hemangioma is a type of birthmark that results from malformed blood vessels. This type of birthmark is often removed by laser surgery.
Home care
Some skin lesions can be very itchy and painful. Home remedies may be an option. Lotions and oatmeal baths can be used to relieve itching caused by skin lesions.
Most wounds take between 1 and 3 weeks to heal. Laser surgery may cause your skin to change color, but then gradually return to its original color. Sometimes you will only need a bandage. Other times, you might need stitches.
Contact dermatitis is caused by friction between the skin and clothing. Absorbent powders or protective balms are available to reduce friction and prevent further skin lesions.
Summary
You can have skin lesions from birth, or they may develop throughout your life. Secondary lesions are skin lesions that become more severe or irritated over time. Skin lesions can also be caused by friction, allergens, or other external irritants. You may also develop lesions as you age or from chronic conditions.
Some lesions can be treated at home with creams and topical ointments. Some lesions require medical attention. It is best to consult a doctor if you are not sure what kind of lesion you have.